Role of the abdominal muscles and changes during pregnancy
The abdominal muscles keep your internal organs in place as well as supporting your spine. In pregnancy they also support your growing baby and uterus. The abdominal muscles and ligaments stretch throughout pregnancy under the influence of the hormones Progesterone and Relaxin.
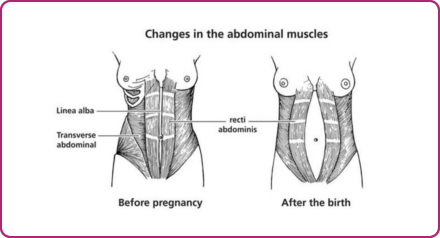
The Rectus Abdominus muscles pass from the ribs and breastbone to the pubic bones. They are the most superficial of the abdominal muscles. Below them are the Oblique muscles and Transverus Abdominus. A ligamentous band called the Linea Alba holds the Recti together. This band softens and stretches as the abdomen enlarges during pregnancy and allows the Recti to move apart. This separation is called a Divarication of the Recti or a Diastasis Recti. It will be checked postnatally by your midwife or physiotherapist and you will be offered outpatient treatment if the separation does not resolve itself quickly and is found to be 3cms or more.
Treatment
After the birth of your baby, your abdominal muscles will feel weak and stretched. As Relaxin and Progesterone start reducing, your muscles and ligaments will gradually become toned.
In the first six weeks avoid movements which may prevent the separation recovering such a, sitting straight up when getting out of the bath or bed and/or heavy lifting.
There are two gentle exercises we suggest to strengthen the deep stabilising muscles whilst the Linea Alba recovers. These can be done in lying, sitting or standing position.
Pelvic floor exercises
The pelvic floor is like a hammock/sling of muscles suspended from inside the front of your pelvis to the coccyx (tailbone). They work with the deep abdominal muscles (Transversus Abdominus) so when you work your pelvic floor the Transversus Abdominus muscles also work.
Try to exercise your pelvic floor at least three times a day in sitting, standing or lying position.
The action is to squeeze and lift the pelvic floor muscles by squeezing and drawing up the back and front passages as though you are trying to control wind and the flow of urine.
There are two ways to work them:
- Hold for several seconds and repeat several times. Aiming to build up to a 10 second hold 10 times.
- Squeeze and lift then let go quickly. Aim to repeat up to 10 times.
Each time you exercise, the muscles become stronger and more supportive. You should also get into the habit of contracting your pelvic floor muscles before lifting, coughing, sneezing or bending.
Transversus Abdominus exercise
Take a breath in, and then as you breathe out gently draw in your abdominal muscles below your tummy button (imagine you are taking in a notch in a low sung belt). Hold this for 5-10 seconds whilst breathing normally. Repeat 5-10 times resting between each pull-in. Try to do this exercise several times a day in sitting, side-lying or standing. They work with the pelvic floor muscles so you could do them together. It is also important to use these muscles functionally so when you are going to pick up your baby remember to gently pull them in.
Your physiotherapist will check your progress and monitor the gap between the muscles before giving you other abdominal exercises to practice. The physiotherapist may also fit you with some elasticated abdominal support in order to encourage Linea Alba to recover if it is felt needed.