Ask three questions
Preparation for your appointments
We want you to be active in your healthcare. By telling us what is important to you and asking questions you can help with this. The three questions below may be useful:
- What are my options?
- What are the possible benefits and risks of those options?
- What help do I need to make my decision?
If your arthritis is not well controlled on conventional synthetic disease modifying anti-rheumatic drugs (csDMARDs), your treatment may be escalated to either a biologic disease modifying anti-rheumatic drug (bDMARD or biologic) or targeted synthetic disease modifying anti-rheumatic drug (tsDMARD) by your rheumatology clinician.
One of the Rheumatology Specialist Nurses or the Specialist Pharmacists will already have discussed with you which medicine you will be taking.
This page has been created to help you remember the important key information in relation to your medicine.
Contents
Section 1 - Choice of treatments
Section 2 - Monitoring
Section 3 - Infections
Section 4 - Vaccinations
Sections 5 - Pregnancy and breastfeeding
Section 6 - Surgery
Section 7 - Side effects
Section 8 - Dose reduction
Section 9 - Home delivery and self-administration
Section 10 - Travel
Section 11 - Contact information
1. Choice of treatment
What are bDMARDs?
bDMARDs are a group of medications that are used to treat arthritis (such as rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis).
These medicines can decrease the amount of inflammation you have and reduce the damaging effects of your arthritis on your joints.
There are now quite a few bDMARDs available to treat different types of arthritis; which medicine you have been prescribed may depend on the type of arthritis that you have or another medical condition at the same time as your arthritis that might make one treatment more appropriate than another.
At the time of writing, bDMARDs used for different conditions include:
- abatacept
- adalimumab
- anakinra
- belimumab
- certolizumab pegol
- etanercept
- golimumab
- guselkumab
- infliximab
- ixekizumab
- risankizumab
- rituximab
- sarilumab
- secukinumab
- tocilizumab
- ustekinumab
However more are becoming available very often.
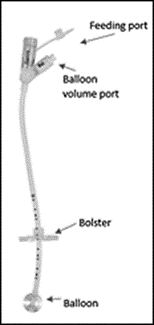
bDMARDs can be given either as an injection into the layer of fat just underneath the surface of your skin (a subcutaneous injection) or by a drip into your vein (intravenous infusion).
If you have a subcutaneous injectable medication you can be taught how to do this yourself at home or someone can be taught to give you the injections, such as a family member.
If you are having an intravenous infusion you will need to come to the Medical Day Care Unit in Southmead Hospital which is located on Level 1 in Gate 5 of the Brunel building.
What are Biosimilar Medicines?
Some of the bDMARD medicines listed above are now available in the UK as similar versions made by different companies, because the patent (allowing one company to make the product exclusively) has expired.
These different versions of existing bDMARDs are known as ‘biosimilars’ because they are deemed to be sufficiently similar (in terms of safety and effectiveness) to the original product.
Switching between biosimilar brands should not affect the safety or the effectiveness of your medicine.
Switching patients to the most cost-effective version of bDMARD allows the NHS to treat more patients with these expensive therapies.
NHS England may ask us to change the brand of bDMARD medication you are prescribed from time to time and we will discuss this with you.
What are tsDMARDS?
tsDMARDs are targeted synthetic therapies.
Like biologic medicines, they target specific parts of the immune system, however they are not made from living cells. They are smaller chemical drugs and can usually be taken by mouth.
There are now quite a few tsDMARD medicines available to treat different types of arthritis; which medicine you have been prescribed may depend on the type of arthritis that you have or your other relevant medical conditions.
At the time of writing, this group of medicines include:
- apremilast
- baricitinib
- filgotinib
- tofacitinib
- upadacitinib
But others are going through approval steps so may be available soon.
How do we help you decide which b/tsDMARD is the best for you?
When your consultant or clinician decides it would be appropriate to start a b/tsDMARD therapy, we will usually invite you to a clinic appointment with the Rheumatology Specialist nurse or Rheumatology Specialist Pharmacist to carry out your baseline assessments (this usually includes a joint examination and blood tests) and talk to you about your new treatment options.
The Nurse or Pharmacist will complete some paperwork with you and discuss the main symptoms associated with your condition, your other medical problems, previously tried therapies and any patient preferences you might have.
Once we have discussed your condition and preferences, we will look at the most cost-effective treatment to suit your needs.
We will support you to make a shared, informed decision about the most appropriate treatment for you.
2. Monitoring
Will I need any special monitoring whilst taking a b/tsDMARD?
This depends on whether you take another medication, such as methotrexate, with the b/tsDMARD medicine.
If you are taking another medication with the b/tsDMARD medicine
If you are taking another medication with the b/tsDMARD medicine
You should be having regular blood tests via your GP to monitor this, and you will not need any different or additional blood tests (unless we tell you). You need to phone your GP surgery to arrange these blood tests.
If you take the b/tsDMARD medicine on its own (monotherapy)
- We usually ask you to have blood tests for full blood count, liver function and kidney function every 3 months for the first year and then every time you are seen for a review by the Rheumatology Team (usually every 6 months).
- For some b/tsDMARDs, the monitoring schedule might be different to this and we will tell you if this is the case.
- If you have a remote consultation (e.g. telephone or video review), we may arrange for you to have your blood sample taken at your GP surgery, but we tell you and advise how we will check the results.
- We may ask you to contact our rheumatology advice line (by email or telephone) to let us know you have had your blood sample taken so we can look out for the results.
- We need to review your blood test results before prescribing your medicines. We will not be able to prescribe your medicines if you have not had your routine blood test.
Will I need to be seen in the hospital clinic for regular reviews whilst taking a b/tsDMARD?
Once you have started treatment, we will usually give you a call after a couple of months to see how you are getting on with your new medication. We will then invite you to attend a face-to-face appointment to check your joints and see if you are responding to your new treatment. This appointment will be either 3, 4, 5 or 6 months after starting treatment, depending on which treatment you are on.
You will then be followed up routinely every 6 months.
Your review appointments may be face to face or in our Remote Therapy Clinic (RTC). This can be via telephone, video, or occasionally we may be able to complete a virtual review which means we have checked your hospital records and blood tests and have deemed it safe to prescribe further medication without speaking to you, but we will always write to you to let you know if this is the case.
If you feel you need to be seen sooner than your scheduled appointment or if you feel you need to be seen face-to-face rather than remotely, please contact us via the rheumatology advice line; you do not have to wait until your scheduled appointment.
It is very important that you do attend regularly for reviews with your Rheumatology Team as the prescriptions of the b/tsDMARD medicines are based on your hospital appointments – if we do not review you in clinic (face-to-face or remotely), we will not be able to prescribe more b/tsDMARD medicine until we have seen you.
It is really helpful for us to understand how you are responding to your b/tsDMARD medication.
Some patients are able to track their symptoms, disease activity and overall wellbeing on a disease activity tracking smartphone application. If you are not already using this but are keen to do so, please contact our rheumatology team so we can register you for this service (free of charge).
If you are expecting to be seen by the hospital but do not receive an appointment letter, please get in touch with us to check you have been booked into an appointment.
What happens if my new b/tsDMARD treatment doesn’t work?
It usually takes about 3-6 months for your b/tsDMARD to be fully effective, although some patients feel the benefit much sooner. We might prescribe you some other medication to help with symptoms whilst waiting for your b/tsDMARD to have an effect.
If your new medication doesn’t help improve your symptoms, we may need to stop your medication, allow for it to come out of your system and decide on an alternative treatment.
Sometimes, your medication will work very well at the beginning but might lose effect over time. If this happens, we may need to stop your medication, allow time for it to come out of your system and chose an alternative treatment.
It is important that you attend your follow up appointments so we can check how well your medication is working. Please always be honest with how your symptoms are feeling.
3. Infections
When not to have your b/tsDMARD and managing infections
You should not have your b/tsDMARD medicine if you are unwell in any way, if you are currently taking antibiotics or if you have just had or are having any surgery in the next few weeks.
You can use the checklist below to help you to decide if it is safe for you to give the injection or to help you decide if you should contact us for further advice before your infusion.
Do you have any of the following?
- Sore throat
- Cough / cold
- Diarrhoea and/or vomiting
- High temperature
- Burning or stinging when passing urine
- Wounds or cuts that could be infected
- Flu type symptoms
- Feeling out of breath
- Dental treatment such as a tooth extraction or a root canal filling.
- Having an operation – see surgery section below
If you say ‘yes’ to any of the above you should contact us on the rheumatology advice line for further advice before giving your injection or before attending your next appointment for an infusion.
After an infection
It is usually safe to restart your b/tsDMARD medication when you are feeling well and you do not have any signs of symptoms of an infection.
If you have had antibiotics
We recommend not starting treatment until at least 48hrs after completing the course of antibiotics as long as you are well.
If you restart your b/tsDMARD therapy on a different day to your usual injection day, this will become your new injection day and you need to count the dosing interval from this day. Never shorten the gap between doses.
If you develop chicken pox, shingles or come into contact with someone who has chicken pox or shingles (and you have not had it before), stop your b/tsDMARD and seek medical attention.
4. Vaccinations
Can I have any vaccinations whilst taking a b/tsDMARD?
- Whilst you are taking a b/tsDMARD medicine you cannot have any live vaccinations, such as the yellow fever vaccination.
- Your GP or practice nurse can discuss the possible risks and benefits of any vaccinations with you and advise which vaccinations are live.
- If you are in your 70s and are offered the shingles vaccination, please check with the GP surgery that they are offering the non-live shingles vaccine which is safe for you to have. You cannot have the live shingles vaccine.
- The yearly flu vaccination, 5 yearly pneumonia vaccination and Covid vaccinations are not live and do not interfere with b/tsDMARDs. We recommend you have these when offered.
5. Pregnancy and breastfeeding
Can I plan for pregnancy and can I breastfeed whilst taking a b/tsDMARD?
Although we have more information to suggest some bDMARD therapies are safe to use in specific trimesters of pregnancy, it is generally advisable that you do not become pregnant whilst on a b/tsDMARD medicine unless you have discussed this with your rheumatology consultant first and been told it is safe to continue taking your medicine.
- Your rheumatology consultant will be able to discuss which treatment is most recommended for your individual circumstances and when the treatment needs to be stopped (or whether you require it to continue).
- This will also impact whether or not your baby can have live vaccines between birth and 6 months old. Generally, you should make sure that you use reliable contraception whilst taking a b/tsDMARD medicine.
- If you unexpectedly become pregnant whilst taking a b/tsDMARD, please discuss this as soon as possible with your rheumatology consultant.
- Some of the established bDMARD therapies can be continued during breastfeeding, but again this needs to be discussed with your clinician.
Can I father children whilst on b/tsDMARDs?
Although it is thought that a number of therapies can be considered safe in men who wish to father children, it is advisable that you discuss this with your rheumatology consultant first and check it is safe to continue taking your medicine.
This decision is made on your personal needs and your thoughts and beliefs are taken into consideration before making the decision; this is to make sure that any decision made is the best one for you and your family.
You should make sure that you use reliable contraception whilst taking a b/tsDMARD medicine.
6. Surgery
What happens if I need surgery?
For planned surgery
You will need to come off your treatment for a certain amount of time beforehand to lower your infection risk with your surgery. Please contact us on the rheumatology advice line well in advance if your surgery so we can advise on the appropriate time to stop your b/tsDMARD.
For emergency surgery
It is important you let the surgical team know when you last had your dose of b/tsDMARD in case you need some preventative antibiotics.
You should also carry your b/tsDMARD alert card around with you.
Following surgery
You can usually restart your b/tsDMARD when your wound shows evidence of healing, any sutures/staples are out, there is no significant swelling, redness or drainage and there is no ongoing nonsurgical site infection, which is typically around 14 days.
7. Side effects
What should I do if I get side effects from my medication?
The information leaflet provided with your medication will list the potential side effects with your specific b/tsDMARD and some information on the likeliness of them occurring.
- Generally, the most common side effects are changes to your blood tests (which is why we monitor them) or increased frequency or severity of infections (which is why it is important that you don’t inject if you have an infection – see when to not have your injection section).
- There is no conclusive evidence to suggest an increased risk of cancer with bDMARDs, but data regarding risk of skin cancers are less clear and we recommend using a high SPF sun cream with UVA/B and 5* rating.
- If you are on a tsDMARD, it is important to report any signs or symptoms of a blood clot, for example chest pain, breathlessness, coughing up blood, leg pain, tenderness or swelling in your thigh or calf.
- You may experience injection site reactions to medicines you inject yourself. Applying a cold compress can help. Usually this reduces when you get more experienced at injecting. If you have a severe injection site reaction or a reaction hasn’t gone away when you are due to inject again, please get in touch with us as you may need to stop your treatment.
- Once you have had your first dose of b/tsDMARD, it is important that you let your GP surgery know you have started your treatment in case you have any reaction to your first or subsequent doses.
- It is important you let you Rheumatology Team know if you are suffering with side effects to your medication.
- If you develop any anaphylaxis or severe side effects, stop the medication and seek urgent medical attention (e.g. contact the usual out of hours emergency medical care).
8. Dose reduction
How long will I be on my b/tsDMARD medication?
- If you are responding to treatment with low disease activity or in remission after being on treatment for two years, we might look at reducing some of your medication.
- Firstly we would want to stop any remaining steroids and make sure you are on the optimal dose of csDMARD.
- We would then invite you to consider our dose reduction program known as Biologics Treatment Reduction by Interval Management (BTRIM). This is a step-wise dose reduction program.
- We will recommend slowly stretching out the gap between your injections in a very controlled way and allow you to decide when you are ready to stretch the gap out further or decide if you need to go back to the previous effective dose.
- We will provide you with written information about this and clears steps of action to take if your symptoms worsen.
- We will not supply you with less medication when you are trialling dose reduction so you will be able to return to standard dosing if preferred.
- Not all patients are able to come off treatment completely but many patients are able to stretch out the gap between their injections to reduce their overall dose.
- If you are keen to reduce the dose of your medication after 2 years on treatment and this hasn’t been discussed with you, please speak to your clinician at your appointment.
9. Home delivery and self-administration
Additional information for self-injectable bDMARDs and oral tsDMARDs, supplied by home delivery
The rest of this page focuses on the important parts to remember if you are taking an injectable form of bDMARD or oral tsDMARD medicine that is supplied via a home delivery provider.
How do I get supplies of my medicine?
Your b/tsDMARD medicine can only be prescribed by your Rheumatology team through the hospital. This means that you won’t be able to collect it with your usual medicines from your pharmacy, chemist or GP.
We use a Home Delivery Service who will deliver your medication to you at home. If you wish, you may arrange with them to deliver your medication to an alternative address (e.g. work address) if this would be more suitable (but this cannot be a local GP or community pharmacy).
Your Rheumatology Specialist Nurse or Specialist Pharmacist can give you details about which home delivery service will be delivering your medication.
Do my medicines need to be stored in the fridge?
- bDMARDs generally need to be kept in the fridge (between 2-8°C).
- Occasionally they can be kept out of the fridge for a short duration (depending on which injection you use).
- When you receive delivery of your first injections, they should be put in the fridge and until you are informed that a nurse is coming to show you how to inject your first dose.
- We recommend taking your injection out of the fridge 30 minutes before you inject it to reduce the change of it stinging when you inject it.
- tsDMARDs do not need to be kept in the fridge.
What happens if a bDMARD (biologic) medicine is left out of the fridge for too long or the fridge breaks down?
If this happens then you will need to contact the homecare delivery company who deliver your medicine and let them know so that they can arrange for the affected medication to be replaced.
You will also need to let the Rheumatology department know by calling the rheumatology advice line in case we need to provide the homecare delivery company with another prescription.
In some circumstances, we may advise that one or two injections can still be used, but we will provide personal instructions to you depending on your situation.
tsDMARD medicines do not need to be stored in the fridge.
What happens if I forget to give an injection or take a tablet?
If you forget to give an injection then you should give a dose as soon as you remember and then make sure that you take the next dose at the correct interval to make sure that you do not give the next dose too early.
For further advice on the specific medicine you are taking please contact the Rheumatology Advice Line.
If you forget to take a tablet (tsDMARD), do not take a double dose to make up for the forgotten dose. Take your next tablet at the usual time and continue as before.
What happens if something goes wrong when giving an injection (bDMARD)?
If the pen or syringe slips when you are giving your injection or if the device does not work properly for any reason please contact us on the Rheumatology Advice Line for more help on the particular problem you have experienced.
Do not try and inject another dose in case some of the first dose was given.
What should I do if the pen or syringe is faulty?
If you think that your pen or syringe is faulty for any reason please make a note of the batch number and expiry date (this information can be found on the box containing your medicine).
Please report any faulty pens or syringes to your home care delivery company.
How do I dispose of my injections?
You will be supplied with a sharps bin for disposing of your injections. When your sharps bin is full with used pens/syringes, contact your homecare company to arrange a collection for disposal.
10. Travel
Can I take my biologic/tsDMARD medicine on holiday with me?
It is possible to travel (either abroad or within the UK) with your b/tsDMARD medicine, but you will need to plan ahead.
- Airlines – ask your airline company in advance whether you can carry your medicine in your hand luggage (do not place your medicine in any checked in luggage as the baggage area is too cold).
- Carry documentation with you to explain why you need to take the medicine with you. You can ask the home delivery company to provide you with a letter for this purpose and we recommend taking your most recent clinic letter with you. You can also call us on the rheumatology advice line if you are struggling to get the suitable letter. Please make sure that you allow enough time between letting us know and us being able to post the letter to you before you travel.
- As a general rule, all biologic medicines should be stored in a refrigerator at temperatures between 2 and 8°C. Please contact us on the Rheumatology Advice Line for advice on how to safely transport your individual medicine.
- Please let us know in advance if you are planning to travel, so we can make sure you have sufficient supplies of medication.
- We can also provide extra advice about reducing the risk of infection when travelling.
11. Examples of who to contact
Contact your homecare provider
If you:
- have any problem with deliveries
- run out of supplies
- leave medication out of the fridge by mistake (you will also need to contact the rheumatology advice line)
- have a faulty pen or syringe
- have a full sharps bin that needs collecting
- need to change your delivery address
Contact the rheumatology advice line
If you:
- have any questions about your medication
- have any side effects
- have run out of medication and your homecare provider are telling you they do not have a prescription
- are unsure whether you should have your b/tsDMARD (e.g. if you feel unwell)
- feel you need to be seen sooner than your scheduled appointment or would like to change a remote consultation to be seen face-to-face
- leave medication out of the fridge by mistake (you will also need to contact the homecare provider)
- are expecting to be seen by the hospital but have not
- received an appointment letter
- want to plan a pregnancy
- feel your medicine has stopped working
- you are planning a holiday
Contact your GP
To arrange your blood tests and let them know once you’ve had your first dose of b/tsDMARD.
Contact emergency care (e.g. GP, 111, A&E)
If you have an allergic reaction to your medication or severe side effect.
Glossary of Terms
Subcutaneous injection
An injection using either a syringe or a pen injection device. The injection is given into the small layer of fat just underneath the surface of the skin.
Intravenous infusion
Medication which is given slowly through a needle in your vein.
Biosimilar medicines
These are different versions of existing biological medicines, thought to have similar effectiveness and safety, brought out because the patent (allowing one company to make the product exclusively) has expired.
Monotherapy
This is a term which is commonly used when patients have just one medicine to control their arthritis.
Dental extraction
Removal of a tooth, which would leave a hole in the gum and may become infected.
Root canal filling
Filling material is placed in the canals and the tooth is sealed with a temporary filling to protect it from infection. Then a crown is usually placed over the tooth to seal and protect it from recontamination and future damage.
References
www.medicines.org.uk
www.rheumatology.org.uk
www.versusarthritis.org/about-arthritis/
How to contact us
Rheumatology Advice Line
Telephone: 0117 414 0600
NHS Out of Hours Service
111 (Monday to Friday, 6.30pm - 8am, all day weekends and Bank Holidays)
Rheumatology Advice Line
rheumatologyadviceline@nbt.nhs.uk
Living With app
Contact the rheumatology advice line to sign up.