Ambulatory Electroencephalography (aEEG)
Please read this information carefully before coming in for your Ambulatory Electroencephalography (aEEG).
What is an ambulatory EEG?
EEG stands for electroencephalogram. Ambulatory monitoring involves recording the electrical activity in your brain when you are going about your normal daily activities, meaning you leave the department with the electrodes attached. This recording is usually done for 48 hours.
What does an ambulatory EEG involve?
An ambulatory EEG recording involves coming to Southmead Hospital for 3 separate appointments, 3 days in row.
What happens during an ambulatory EEG?
Your first appointment
This appointment will take around 60 minutes.
- Your head will be measured, then rubbed gently and 23 small metal discs will be applied to your head with soluble sticky paste, before being firmly attached with Mavidon glue.
- 2 electrodes will be applied to your shoulders to measure your heart rate during the EEG.
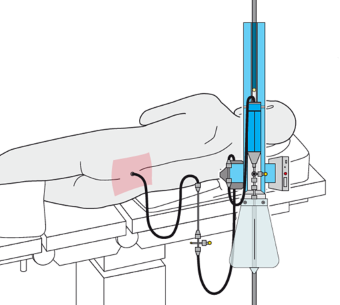
- These discs will then be attached to the small recording box with wires.
- The box will stay attached to you for the duration of the test and can be carried in a bag over your shoulder.
- You will be given a diary to complete. You will need to give a basic outline of your daily activities (eating, sleeping etc) as well as any typical events.
- We will also ask you to press a red event button, which is attached to the recorder, if you have any of your typical events. If you have no recollection of your events happening, it could be useful to have someone stay with you overnight to help you fill in the diary.
Your second appointment
This appointment will take around 30 minutes.
- You will need to bring your diary sheet back. The information on the recorder will be downloaded, the batteries will be replaced and all discs will be checked.
Your third appointment
This appointment will take around 60 minutes.
- The discs will be removed with acetone and as much glue as is possible will be removed, but you may still find loose bits in your hair.
- Use conditioner and a fine comb at home to help remove the final bits of glue.
Preparing for the test
- You must arrive with clean, dry hair with no grease, gel, wax, or other hair products - these can impair electrode/skin contact. You will not be able to wash your hair until after the electrodes are removed on the third day.
- Wear clothing which is loose fitting around the neck, preferably an open neck shirt/blouse with button fastening or a wide necked T-shirt. This will make it easier to undress when going to bed.
When will I get my results?
You will not get your results straight after the test or see a doctor on the day, as the ambulatory EEG needs to be fully analysed.
A full report will be sent to the GP or consultant who referred you within 2 weeks, they will then contact you to discuss the results. Please note, results are not sent directly to you.
Contact details
This information is intended as a guideline only. If you have any further questions about your test (excluding about results) please contact the department on the numbers below and a member of staff will be happy to help.
Your responsibility as a patient
Outpatient services at North Bristol NHS Trust are in great demand. Even so, every week an average of 600 patients fail to attend, which wastes appointments. Please tell us with as much notice as possible if you no longer need your appointment and we can allocate this to another patient.
What if I am unwell or need to change my appointment?
If you have an infectious condition, such as COVID-19, measles, mumps, chickenpox, flu, stomach upset, have head lice, or are unable to attend your appointment for any other reason, please let us know with as much notice as possible so that your appointment can be rescheduled and offered to someone else.
If you want to change the appointment for a second time, we cannot offer you another date unless there are exceptional circumstances.
What if I don’t attend?
We will assume that you no longer require your appointment, and we will not offer you another one. We will write to the consultant/doctor who referred you and inform them that you did not attend.
© North Bristol NHS Trust. This edition published December 2024. Review due December 2027. NBT003736
Support your local hospital charity

See the impact we make across our hospitals and how you can be a part of it.