Parvovirus B19 during Pregnancy
Parvovirus B19 is also known as Slapped Cheek, Human parvovirus or Fifth Disease.
What is Parvovirus B19?
Parvovirus B19 is a virus that commonly infects children. It is usually transmitted by coughing and sneezing (respiratory droplets). Hand washing is important in helping to prevent spread. School teachers, childcare workers and mothers of young children are particularly likely to be exposed to this virus as it is commonest amongst younger school age children, but everyone can be exposed to it.
For most healthy people, Parvovirus B19 causes a mild, self-limiting illness which is followed by life-long immunity.
The Human Parvovirus B19 is not the same Parvovirus that vets may be concerned about in pets, especially dogs, and it cannot be passed from humans to animals or vice versa.
Pregnant women are not routinely screened for past parvovirus B19 infection as there is no vaccine or preventative treatment available.
How common is Parvovirus B19?
The exact number of Parvovirus B19 infections in the UK is not known as the virus does not always show symptoms, and the diagnosis can only be confirmed by blood test.
- Parvovirus B19 infection is common in developed countries — about 15% of pre-school children, 50% of adults, and 85% of elderly people show evidence of past infection in their blood.
- Infection with Parvovirus B19 can occur at any age, but is most common in children aged six – ten years.
- One in 512 pregnancies may be affected.
- Seasonal outbreaks of Parvovirus B19 occur every three – four years in the UK, mainly in late winter and early spring. During school outbreaks, ten – 60% of exposed children develop symptoms consistent with Parvovirus B19 infection.
What are the symptoms of Parvovirus B19?
Parvovirus B19 commonly causes:
- High temperature
- Mild cold-like symptoms including feeling under the weather, a sore throat and a runny nose
- Headache
- Mild nausea and /or diarrhoea
The symptoms may happen several days before a rash.
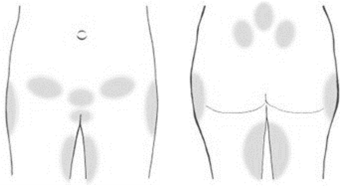
- The rash is the result of your immune system reacting after the infection has passed. The rash is often present on the face in children and looks like a ‘slapped cheek’ appearance. Facial rash is uncommon in adults. The rash may extend down to the chest, arms, stomach and thighs. It has a lace-like appearance and can sometimes itch. It may take a few weeks for the rash to completely clear and during that time it may seem to worsen until it fades away entirely. Certain stimuli e.g. heat, exercise and anxiety or stress may reactivate the rash until it completely fades. In some cases, especially in adult women or older teenagers, joint swelling or pain may occur.
- Rarer symptoms may include swollen glands, red eyes, sore throat, and a rash that might look like blisters or bruises.
A person with Parvovirus is infectious seven to ten days before the rash (if any) develops, until one day after the rash appears. Exposure to infection with Parvovirus B19 may have occurred earlier than you think.
It is important to note that many people (up to 30%) with Parvovirus B19 have no symptoms at all. Less than 50% have a rash.
Why should parvovirus contact or infection be investigated in pregnancy?
In women who are not immune, infection in the first 20 weeks of pregnancy can lead to serious problems for your baby before it is born. This would usually happen three to five weeks after the onset of maternal infection, but can be later.
Most women who have parvovirus in pregnancy will have healthy babies.
Parvovirus B19 is not known to cause congenital abnormalities. However, the infection can be passed from mother to baby and may cause the baby to become anaemic. The level of anaemia and the length of time the baby might have anaemia will be variable and unpredictable. The health of your baby can be monitored to check for signs of anaemia.
The greatest period of risk to the baby is between four to 20 weeks. Infection during this time can sometimes lead to serious complications such as fetal anaemia and sometimes fetal loss (miscarriage or stillbirth). There is a five – ten per cent risk of fetal loss if women develop this infection in the second trimester.
Infection in the first month of pregnancy is not thought to carry any risk.
After 20 weeks of pregnancy the risk of the baby developing severe anaemia is much lower but investigations are undertaken in all cases.
It is important to remember that most babies will not be infected or affected by the virus.
What happens if I think I may have been in contact with Parvovirus B19?
If you have think you have been in contact with Human Parvovirus B19 infection or if you have a rash you should urgently report this to your midwife or doctor as you will need to have a blood test.
Contact is defined as being in the same room as an infected person for a prolonged period (15 minutes or more) or face-to-face contact with the person. The main source of infection in pregnancy is from household (rather than occupational) exposure.
Until parvovirus infection has been ruled out you should avoid contact with other pregnant women to reduce the risk of infecting others.
The blood test will tell you if:
- You have had Human Parvovirus B19 infection before and are now immune and not at risk of infection as you have antibodies to protect you from infection. *Parvovirus B19 is common and 50-60% of adults have evidence of past infection.
- You currently have Parvovirus B19 infection.
- You have not had Parvovirus B19 infection before and are at risk of infection.
- The blood sample may also be tested for rubella (German measles) in the same way it looks at your parvovirus status if you have no record of previous rubella testing or MMR immunisation.
If I have had a blood test for Parvovirus B19 how soon can I expect my result?
If your midwife or doctor has taken a blood test for Parvovirus B19 infection the result should be available within six working days from sample arriving in the laboratory. Your midwife or doctor should contact you with the result as soon as they receive it.
If you do not hear from your midwife or doctor by seven working days after the test it is strongly advised that you contact them or the surgery, health centre or the Antenatal Clinic of the hospital stated on your maternity yellow book.
If your results show you are Parvovirus B19 antibody negative you are at risk to infection by Parvovirus B19. You will be re-tested one month after the last date of contact to see if you have developed antibodies to the virus. This is to ensure unrecognized (no symptoms) infection is not missed. You should report any rashes that occur in pregnancy or any further contact with known infection as you may need to have another blood test. During this one month you should avoid other pregnant women where possible and inform antenatal services about the contact prior to attending any clinic or ward.
If your initial or follow-up blood test shows you have recently been infected your baby may be at risk of developing the infection. Your doctor and midwife will refer you to a Specialist Fetal Medicine Clinic for further follow-up.
If the results show that you have the infection, you will be referred to a Specialist Fetal Medicine Clinic where you will be offered frequent ultrasound scans to check your baby’s health. An individualised plan for scans is made according to your stage of pregnancy and the findings at each scan. As well as checking the health of your baby, the purpose of the scans is to pick up any signs that your baby is developing symptoms of anaemia.
It is important for you to be aware of the pattern of your baby’s movements and immediately report any changes or concerns to a Health Care Professional.
If the baby shows signs of developing anaemia on scan, an intrauterine blood transfusion may be offered as a treatment for the anaemia. Intrauterine blood transfusion is a process where blood is given to your baby before it is born. This treatment is usually successful in treating anaemia but the procedure itself carries a small chance of miscarriage. If this treatment option is required, the procedure, the benefits, risks and likely outcome will be discussed with you fully by the person carrying out the treatment. The procedure is not undertaken at Southmead Hospital, you will be referred to St. Michael’s Hospital, Fetal Medicine Unit for this.
References & Sources of further information
Fifthdisease.org (2017) What is Fifth Disease
https://www.fifthdisease.org/
[Accessed: 15.11.2017]
NHS (2015) Slapped Cheek Syndrome.
https://www.nhs.uk/conditions/slapped-cheek-syndrome/
[Accessed: 15.11.2017]
NHS (2017) What are the risk of slapped cheek syndrome during pregnancy?
https://www.nhs.uk/chq/pages/1112.aspx?categoryid=54
[Accessed: 15.11.2017]
NICE: National Institute for Health and Care Excellence. Parvovirus B19 infection: Last revised in February 2017
https://cks.nice.org.uk/parvovirus-b19-infection#!scenario:2
[Accessed: 5.12.2017]
https://cks.nice.org.uk/parvovirus-b19-infection#!backgroundsub:1
(Accessed 05/12/2017)