What is pregnancy-related pelvic girdle pain?
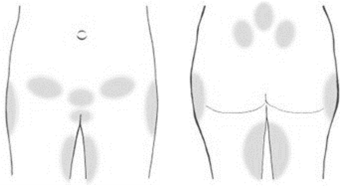
The term ‘pregnancy-related pelvic girdle pain’ (PGP) is an umbrella term to describe the aches and pains around the pelvis during pregnancy. The diagrams below outline all the areas where pain can arise during pregnancy.
For most women the symptoms are mild but for some they can be severe. Although PGP can be painful and distressing, it will not harm your baby.
Pain can arise from the following areas
- Lower back.
- Symphysis pubis joint.
- Sacroiliac joint.
- Groin.
- Front/back of thigh.
- Hip/outer thighs.
- Pelvic floor/perineum.
PGP is common, with 1 in 5 women experiencing pain during pregnancy. This means that you might have pain or difficulty with activities like:
- Walking (especially for prolonged periods).
- Climbing stairs.
- Turning over in bed.
- Putting on socks/tights/shoes/trousers.
- Getting in/out of the car and driving.
- Sex.
Other symptoms of PGP may include clicking or grinding sensations when moving, or feeling that the pelvic joints are loose/unstable. It is important to know that the pelvis is extremely strong and stable, and there is no evidence that the pain you have is a sign of damage.
The good news is that it is pregnancy-related, which means that for most women, the pain quickly improves after giving birth. For around 1 in 10 women, the pain can take a little longer to settle down, and may carry on past the initial post-natal period.
What causes PGP?
There are lots of different factors that contribute to PGP, it is likely a combination of these that cause pain.
You are more likely to experiences PGP if:
- You have had back pain before your pregnancy.
- You have had PGP in a previous pregnancy.
- You start your pregnancy being overweight.
Here are some factors that contribute to PGP:
Hormonal changes
Strong tissues called ligaments hold the bones of the pelvis together. The normal hormonal effects of pregnancy cause the ligaments to be more flexible. This is an important process, and without it you would not be able to grow your baby. This does mean that your joints are more mobile, however research hasn’t shown a link between how mobile your joints are and how much pelvic pain you have.
It is know that sensitivity to pain increases during pregnancy, and this may be a bigger factor in why we are more likely to experience pain.
Postural changes

The average weight gain in pregnancy is two stone, and your pelvis has to accommodate a growing baby. You may have noticed that your posture has changed with pregnancy. Lots of women find the curve in their lower back may become more pronounces as their bump grows.
This is not damaging or harmful, but too much time spent in any posture can cause a feeling of stiffness and be painful. It can be helpful to be mindful of this.
Activity level
Having a job involving manual work/lifting activities or prolonged standing/walking can impact your pain. Our bodies have to adapt to our normal activities whilst carrying an extra load.
Additionally you may not be as active as you were previously so your body will have to adapt to a different routine.
Emotional factors
It is well known that emotional factors can impact the levels of pain we experiences.
Factors such as stress, depression, anxiety, and fatigue all have an influence on the sensitivity of our nervous system, and in turn this can impact pain levels. This means that you may be more likely that you experience PGP if you have any of these, and it is important that you can access appropriate support.
Dealing with factors like morning sickness, fatigue, and lack of sleep can also contribute.
It is likely that you will have an element of pain until you give birth. However the good news is most women recover
completely within the first month following birth, and there are lots of strategies you can use to help in the meantime, which are covered on the following pages.
What can I do to help PGP?
It can be helpful to consider the following 4 Ps to help manage the symptoms:
- Posture.
- Pain relief.
- Pacing.
- Physical exercise.
Posture
Looking after your posture as your body changes during pregnancy can be really helpful.
The best strategy is to change your position regularly, however if you do need to stay in one position for a bit longer, the following advice can help:
- Using a rolled towel or cushion can help to support the lower back when sitting. Gently rocking your pelvis backwards and forwards regularly can help to keep your back moving while you are sitting.
- You could also try sitting on a gym ball periodically, as this also helps to keep you gently active whilst sitting.
- You may find that positions involving standing on one leg can feel uncomfortable. Adapting your posture to reduce this can be helpful - such as getting dressed sitting down, or trying to stand with your weight evenly between your feet.
- At night time, using pillows between your legs can be helpful. Place a pillow between your knees and ankles when lying on your side at night (see picture). When you need to turn, squeezing into the pillows may feel more comfortable.
- A small pillow or towel placed underneath your bump when lying can be helpful.
- Pad out your bed with a spare double duvet placed under your top sheet – this will help to spread the pressure and may stop your hips from getting sore when side lying.
- When getting out of bed, it can be more comfortable to roll onto your side before getting out of bed, keeping your legs together.
It is important to try and be consistent with the above tips. Simple advice done well can often make the biggest difference.
Pain relief
Your GP will usually feel it is safe for you to take regular paracetamol during your pregnancy. Please speak to your GP to discuss this further or if you need advice on stronger pain relief. There are many other pain relieving strategies such as:
- Using heat such as hot water bottles/heat packs as long as you don’t directly apply the heat to your bump. You could also try cold if you prefer – either a cold pack or frozen peas wrapped in a damp towel.
- Using a maternity support belt, tubigrip, or supportive clothing may reduce pain on walking (the softer belts without rigid supports tend to be more comfortable).
- Having a massage from a partner or friend (in a chair or side lying rather than on your stomach).
- TENS (transcutaneous electrical nerve stimulation) machines can also be helpful, and are safe to use from 37 weeks pregnant.
- Concentrating on your breathing when you’re in pain can help, not only if you are experiencing PGP but also in labour. When pain is intense, it’s very easy to start taking shallow, rapid breaths. Instead, try to breathe slowly and deeply. This will help you to feel more in control and can help to ease muscle tension which may make your pain worse.
Pacing
Learning to pace yourself as you progress through pregnancy can be a really useful strategy for managing aches and pains.
Pacing means breaking activities into shorter sections, and planning short rest breaks in between each chunk of activity.
Pacing also means planning your activities so you avoid a ‘boom/bust’ pattern – this is doing a lot of activity on days when you feel good, but then having to spend days resting because you may have overdone it.
Ask and accept help if you need it.
Physical exercise
Exercise is another important part of trying to manage your pain. Keeping active can feel like a real challenge when you’re in pain but it is important to do what you can and to aim for 150 minutes of physical activity each week.
There are some rules to be mindful of in pregnancy:
- Avoid physical activity in excessive heat, especially with high humidity.
- Keep your exercise to a ‘moderate’ level so your heart rate does not raise too much – you should be able to hold a conversation whilst exercising.
- Avoid dehydration and drink plenty.
- Avoid exercise that might risk ‘bumping the bump’.
If you are experiencing pelvic girdle pain then gentler exercises may be more appropriate and feel more comfortable – this could be walking, swimming, or antenatal yoga/pilates.
It is important to listen to your body and pace yourself, and it is recommended from 16 weeks that you do not exercise lying on your back.
We have provided some basic exercise examples in our pelvic girdle pain video:
- What is pelvic girdle pain? (up to 2 minutes 50).
- What can I do to help? (from 2 minutes 50) Information on posture, pacing, pain relief, support belts, heat.
- Exercises you can try (from 9 minutes 50).
PGP, stress, and your emotional wellbeing
Stress, depression, and anxiety can all have a negative influence on your pain, and it is important to recognise that experiencing PGP can affect you emotionally as well as physically.
It can be difficult to remain positive when you have PGP, so it is important to look after your mental wellbeing as best you can throughout your pregnancy.
Incorporating things like relaxation, breathing exercises, mindfulness and yoga have been shown to help anxiety in pregnancy. Your fitness routine might also be part of how you relieve stress.
We have put together some resources at the end of this booklet which you may find helpful.
If you feel like you are not coping, please speak with your health professional for advice. Within Bristol, Mothers for Mothers provide support to help families manage their wellbeing and mental health during pregnancy and after birth.
Their services can either be accessed through self-referral or your healthcare professional can do this for you – their website details are at the end of this booklet.
More useful resources
©North Bristol NHS Trust. This edition published March 2025. Review due March 2028. NBT002884
