(Conservatively managed fragility fracture of the clavicle).
This information is for people who most likely won’t need an operation after breaking their clavicle (collar bone). This means you don’t need to come back to the hospital to see the orthopaedic doctors or have another X-ray in the Fracture Clinic routinely.
Please see the phone numbers at the end of the page if you have any questions or concerns following your injury.
These guidelines work for most people in your situation who have had a similar injury. It will help your recovery if you follow them as best you can. The information can also be used by the people involved in your care for those that are unable to follow the advice on this page themselves.
Summary:
- Ask someone to help during your recovery.
- Wear loose clothing.
- Support your arm either in a sling or on pillows for comfort.
- Take regular pain killers as advised by your doctor.
- Stay well hydrated and take laxatives if needed.
- Monitor the skin over the broken bone – contact Fracture Clinic if the skin becomes inflamed or blistered or broken.
Practical considerations
- You should write down the date you have broken your clavicle.
- You are unlikely to be able to use your arm properly while it is healing so you might need extra help during this time. This can be from family, friends, or you may need extra help from the community support team.
- Consider loose clothing for comfort, ease of dressing and getting to the toilet. A loose shirt for your top half and trousers or skirts with elasticated waists can make a big difference on how you cope at home. Put your injured arm in the sleeve first (and remove last) to reduce pain and unnecessary movement.
- When you are feeling more comfortable and your pain is improving you can use your arm normally to care for yourself– including putting weight through your arm to use walking aids if required.
Supporting your arm
Your sling can gradually be removed as your pain improves. There are various sling options and you may need to experiment to find what works best for you. Please contact the Plaster Room on 0117 414 8606 if you are struggling with your sling.
Some options include:
A full arm sling or ‘Polysling’
This may be most comfortable in the early stages and if correctly applied and tightened regularly can provide good support for the broken bone. It can however be difficult to put this sling on and off by yourself. And it can make it too difficult to use your arm and look after yourself.

A collar and cuff
This sling can be easily adjusted for comfort and is easier to put on and off yourself.
Try to position it so it is supporting the weight of your arm well as pictured.

Walking aids
If you use a walking aid such as a frame you may not need your sling on as the frame will provide the support your arms needs.

Pillows
You can support your arm on pillows instead of the sling when you are sitting down. This will give your neck a rest from the sling.

Pain control
- Your injured arm is likely to be very painful initially. It’s important that you keep the pain under control as much as possible. Please ensure you take regular painkillers as recommended by your doctor. Speak to your doctor if your pain remains poorly controlled.
- Constipation is a common side effect of painkillers and reduced activity. Please try to stay well hydrated and take laxatives if required. It is important to seek advice from a health professional if you remain constipated.
Monitoring your skin
If the bone fragment (where it is broken) is sharp and prominent it can occasionally cause problems with your skin directly above the break. You are likely to have been advised if this is a concern for your break, but occasionally this only becomes apparent after your injury was assessed.
If this is the case, you will need someone (a family member or carers) to closely monitor the skin. If you have any signs of the skin breaking down or infection you must contact the Fracture Clinic for review on 0117 414 1260.
Signs of problems may include:
- Heat, redness, and increased swelling after the initial bruising and swelling goes down.
- Small area of blistering or ulcer type appearance over the bone fragment.
Preventing chest infections
There is an increased risk of developing a chest infection while you are recovering. You are likely to be less mobile than normal and you may also find it hurts when you breathe deeply.
Taking deep breaths can reduce the risk of chest infections by keeping your lower airway working well, and by reducing the build- up of secretions. To help reduce this risk:
- Breath in slowly through your nose, imagine the base of your lungs expanding fully.
- Slowly exhale through your mouth.
- Do this 2 to 3 times in a row.
Try to do this every half hour if you can. You could set a timer, ask a family member or carer to remind you; or if you are watching television, use the adverts as a prompt.
What to expect in your recovery
Using your arm
Please consider that it may be some weeks before you feel comfortable to use your arm effectively.
Eating and drinking
You may need some help to eat and drink initially especially if you have injured your dominant arm.
- Eating ‘finger foods’ such as sandwiches can be easier than food that needs to be cut up.
- There are adaptations such as a ‘plate guard’ (pictured below) or wide handled cutlery that can make it easier to eat. These items are widely available to purchase if required.
- Please ask a health professional if you are struggling and unsure what to do.

Gradually increase the use of your arm as your confidence increases and the pain settles. Trying to use your arm to eat, drink and care for yourself gives you the best chance of a successful recovery.
- Practicing with an empty cup will build your confidence for meal times if you’re struggling to begin with.
- Practice washing your face with your injured arm while sat at the sink. You can use the other hand to help if needed.
Exercises
Keep your fingers and wrist moving – make a tight fist and open your hand fully throughout the day.

Remove your sling and gently extend your arm.
Now bend you elbow and try to bring your hand up towards your shoulder.

Getting your shoulder moving from about 3 weeks after your injury
The following exercises are suggestions. The important thing is to gradually get your shoulder moving in whatever way you feel able to.
You might need help for the following exercises. Please speak to your community therapy team if they are involved in your care to help you with exercises.
Place your hand under the elbow of the injured arm. Lift gently until you feel a stretch at your shoulder.
Start to gradually increase how far you can move your shoulder.

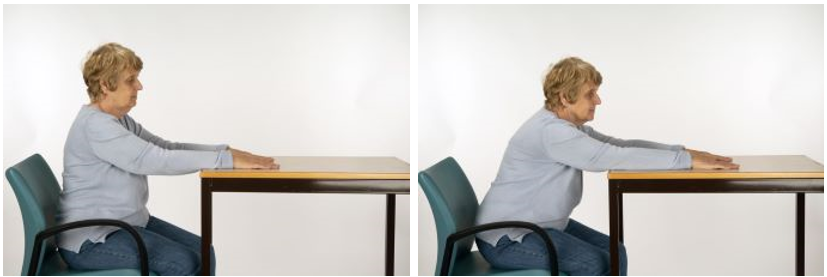
Place your hands on a table. Slide your hands along the table as far as you can without lifting your shoulders.
Bone health and fracture prevention
Bones contain living tissue that is constantly being broken down and rebuilt. We call this process ‘bone turnover’.
As we get older, the process of making new bone is slower than the process of breaking down of old bone, and so the amount of bone tissue we have reduces, and bones can start to lose some of their strength and structure and become weaker. This may lead to a condition called osteoporosis.
A fracture that has happened easily after a minor injury such as a trip or fall is known as a fragility fracture. It is often the first sign that bones have lost some of their overall strength and structure.
People who have had a fragility fracture have a higher chance of having another fracture compared to someone who hasn’t had a fracture.
You may be contacted by the Fracture Liaison Service who will arrange to complete a ‘fracture risk assessment’ to see how likely you are to have further broken bones (fragility fractures). This may also be carried out by the team looking after you in hospital, or your own doctor at the GP surgery.
The fracture risk assessment can help to guide whether you should have some further tests or investigations for osteoporosis. If it indicates that you have a high chance (risk) of having fractures, it may be recommended that you start taking some medication to help slow down the bone turnover process and improve your bone strength. This will help reduce the chances of having significant fractures like a hip fracture or a compression fracture of one of the spinal bones.
What else can you do to keep your bones healthy?
A healthy lifestyle is important to reduce your risk of developing osteoporosis and having fractures, but if your risk for having fractures is high then it might not be enough on its own to reduce your chances of having further fractures.
Exercise is good for bone strength - even if you have osteoporosis, a combination of good balance, coordination, and reflexes can help to reduce your risk of having a slip, trip, or fall.
You may find it beneficial to do some strength and balance training to help reduce the chances of falls and further broken bones in the future. You may have this offered as part of your care support after your injury. If not there are classes and groups in the community you may wish to join, such as the Staying Steady classes but if you have had one or more falls, or if you remain worried about falling, ask your GP to refer you to the specialist Falls Service.
You can also help your bones by not smoking and by not drinking too much alcohol. Smoking, and/or regularly drinking more than the recommended weekly amount of alcohol has a harmful effect on bones, reducing the body’s ability to absorb calcium and changing how bone-building cells work, and can slow down the healing of fractures.
Drinking more alcohol than the recommended safe amounts can also cause people to become unsteady on their feet and increase their chances of having falls and fractures.
You should also make sure you have enough calcium and vitamin D, either from a healthy balanced diet and safe exposure of your skin to sunlight during the spring and summer, or by taking calcium and/or vitamin D supplements.
For further information, you may wish to visit the website of the Royal Osteoporosis Society: Better Bone Health for Everybody (theros.org.uk) or contact their specialist nurse helpline on 0808 800 0035.
How to contact us:
Frailty Trauma Practitioner
07511 166031
Single Point of Access: Sirona community based assessments
0300 125 6789
Plaster room
0117 414 8606
0117 414 8607
Available: Monday - Friday 8:30am - 5pm Saturday, Sunday, and bank holidays 8:30am - 1pm
© North Bristol NHS Trust. This edition published May 2024. Review due May 2027. NBT002391.
