This information has been written by the teams who will look after you during surgery. It aims to help you understand the surgery, guide you through these various phases of your operation, and inform you how you can best prepare and recover afterwards.
You may be given a paper copy of this information which you should bring with you on the day of your surgery.
This page contains the following information:
- Preparing for your operation
- On the day of your operation
- Going home
- Physiotherapy advice
- Therapy advice
A joint replacement operation is done to improve your quality of life, It will hopefully allow you to do some of the things that have become difficult with your joint arthritis.
From the day you are admitted to hospital, the staff involved in your care will work together to assess your needs in preparation for leaving hospital.
We ask you to provide us with all the necessary information that will help with planning your hospital care, and timely discharge as early as possible.
You will need to make the arrangements for your own transport home prior to your admission. If you or your relatives/carers have any concerns about your hospital discharge or transfer, do not hesitate to ask a member of the team.
Discharge Lounge
Where possible, discharge arrangements will be made so you are able to vacate your hospital bed. This may include transfer to the Discharge Lounge; we will prepare you and keep you informed.
The Discharge Lounge is a safe area providing nursing care and regular refreshments and meals, including breakfast, where you can wait to be taken home.
Pathway for recovery
Recovering from joint replacement surgery has changed a lot over the years. We know the sooner we get you up and walking after your surgery, the better your outcomes will be. To help you do this, we have developed a pathway using the expertise of other hospitals in this region and across the country.
This should allow you to get back on your feet sooner and return home to do the things you enjoy.
Returning home as soon as safely possible, even on the same day as your operation
As a result of expert surgery and anaesthetics, and a highly skilled team of doctors, nurses, and allied health professionals, many patients will not need to stay in hospital overnight and will be ready to go home the same day.
This is the usual pathway in many orthopaedic centres across the country, providing an excellent standard of care with very positive results and patient feedback.
However, some patients may not be ready to return safely home the same day and will need a little longer. If this is the case, we would expect you to be able to go home the day after your surgery, or as soon as all treating teams are satisfied.
We will only discharge you once you are recovered and you are able to safely return home.
Managing and understanding the Process
It is important for you to have realistic expectations of having joint replacement surgery. You should have a clear understanding of what to expect at each stage. You must prepare appropriately for your surgery and work with the clinical teams you meet during your care.
Preparation for your operation
Prepare ahead
The weeks leading up to your operation are as important as the operation day itself.
After your surgery, you will either return home on the same day, or stay in hospital for just one night. Therefore, you should plan ahead before your surgery and think about how things might be for you when you return home. You must also attend all your appointments before your surgery date.
Arrange for transport
You should arrange for a family member or a friend to collect you after your surgery. The hospital does not routinely provide transport for your return home.
Assistance for after your surgery
You have probably been living with joint pain for some time before your operation and will already have ways of adapting to certain situations at home. However, when you are recovering from your operation you may also need some extra help with general tasks initially, like cooking, shopping, and cleaning. You must organise this help before your operation date.
To ensure that your return home is successful and safe, you will need to have someone to stay with you overnight post discharge, and for a few days after returning home. This is essential if you are to go home on the day of surgery.
Care agency support
Very few people require professional care support at home. If your personal choice is to have this help, you must arrange this privately.
The NHS can only provide professional care based on specifically assessed needs and cannot arrange convalescent care.
Prepare your home
Preparing your home environment in advance is really helpful for when you get discharged.
For example, you can:
- Freeze some simple to cook meals or have some ‘ready meals’ on hand.
- Move any regularly used items that are heavy, or out of reach, to more accessible places, such as move the saucepans you use frequently up from any low shelves or cupboards.
- Avoid potential trip hazards by removing any loose rugs or obstacles from the floor such as excess furniture or things that would be easy to trip over.
- Make arrangements for someone to care for any pets including walking dogs after your surgery.
Keep fit and healthy
The fitter you are before your operation, the less likely you are to have complications during and after your surgery.
You should seek to make some lifestyle improvements, such as:
- Reduce alcohol intake.
- Stopping smoking.
- Keeping as mobile as possible and exercising.
- Losing weight.
If you have any long term health conditions, you should aim to control these as well as possible before your operation to help prevent any complications and to avoid your operation being postponed.
Check your own blood pressure if you are able to do so or get it checked at your GP. If it is above 160/90 you are likely to require medication and the sooner this is started, the sooner we will be able to go ahead with your surgery.
Similarly, if you suffer from diabetes and your HbA1c has not been checked for 6 months or was over 69mmol/mol the last time it was checked, please arrange to have this checked again, and work with your diabetic adviser to improve it. It is very unlikely that your surgery will be undertaken if your diabetes is not well controlled and your HbA1c is above this value.
Pre-operative assessment
The pre-operative assessment process is important as it helps the hospital plan your care.
You will be asked by the hospital to provide some information about your general health and current medications. You may be asked to provide this information via:
- A computer or mobile app.
- A telephone consultation.
- A video consultation.
- A face-to-face appointment.
This allows us to inform and advise you about your procedure, for example, we can provide you with instructions about medications and fasting times before your operation.
What details will be checked?
At your pre-operative assessment appointments, we will check various medical details, such as:
- Your general health status.
- Your blood pressure.
- Your blood count to see if you are anaemic.
- Your kidney functions.
- How well you are controlling your diabetes.
Medicines
We will also review your medicines. It is fine to continue taking most medicines and to take them on the day of your surgery. However, there are certain medications we may need you to stop taking for a few days before your operation, such as:
- Blood thinning / anti-clotting medication.
- Some blood pressure medications.
We will give you clear instructions if this is needed and tell you when you should start these medications again after your surgery.
Ward staff will inform you of the pain relief that your surgical team have prescribed for you when you leave hospital. This discussion will also include advice about paracetamol and ibuprofen, where we advise patients to source their own supplies if they are able to do so, in line with North Bristol NHS Trust Policy.
Do your physiotherapy exercises
The exercises in the Physiotherapy section of this page should be completed both before and after your surgery. Doing these exercises before your operation will strengthen your muscles and will help you to recover more quickly after surgery.
On the day of your operation
You will be given a specific time to arrive, depending on the time of your operation.
Eating and drinking before your operation
You must follow the instructions about fasting times. It is important that you follow the fasting instructions correctly or your operation may be cancelled on the day. You must not have any food or very milky drinks for 6 hours before your surgery.
We encourage you to continue to drink plain water until you arrive at hospital and after your admission this will be provided according to your anaesthetist’s instructions.
What to bring with you to the hospital
- All your current medication in original packaging.
- Wear loose, comfortable day clothes to get dressed back into after your operation. Your leg may be swollen after your surgery so make sure this is an appropriate size.
- Flat, sturdy footwear with a back in it. No mules or sliders.
- Overnight bag in case you are not ready to return home on the same day.
- Glasses, hearing aids, walking aids, or dressing aids that you might have.
- Phone, charger, headphones, music devices, if you would like to listen to music during your operation.
- It is also a good idea to bring something to read or to keep you occupied in case you have a wait. Wi-Fi coverage can be variable.
- Contact details of the person who will be picking you up.
- Any letters you receive from the hospital giving you arrival instructions for the day of surgery.
Please try to avoid bringing in a large number of items with you and minimise items of high value or cash.
Arriving at the hospital
When you arrive, you will be greeted by a member of the reception team. They will book you in and confirm some details with you. You will then be seen by one of the nursing team who will run through some additional questions.
Confirming your consent form
The surgical team will confirm with you the operation that they are planning to perform, and check your consent form. They will use a pen to draw an arrow on the leg that is going to be operated upon.
They will be able to answer any last-minute questions you may have.
Meeting your anaesthetist
Before your operation, you will meet your anaesthetist. They will explain the type of anaesthetic that is going to be used, and answer any questions you may have about the anaesthetic.
Getting ready for your operation
When it is time for your operation, you will be asked to change into a theatre gown. You will then walk to the operating theatre with one of the team. There, you will be greeted by your anaesthetist, and you will also meet the operating department practitioner, who works with the anaesthetist, helping to look after you.
Routine checks
Some routine checks will be carried out to confirm your identity and to check if you have any allergies. We will confirm again your operation, and what side you are having it on.
Attaching monitoring equipment and a drip
One of the team will attach some standard equipment to monitor your heart, blood pressure, and oxygen levels while you are having your anaesthetic and operation.
Your anaesthetist will also be giving you various medicines through a drip in the back of one of your hands. These include antibiotics, anti-sickness medicines and fluids.
Spinal anaesthetic
In most cases, your anaesthetist will give you a spinal anaesthetic. This is very safe, and avoids the need for having a general anaesthetic, which may cause unpleasant side effects.
Spinal anaesthetic also helps you to recover quickly and receive the best post-operative pain relief.
Local anaesthetic is placed around some of the nerves in your lower back. This numbs your pain nerves so that you do not feel pain during the operation.
The operation
Once you are in the operating theatre, your leg will be painted with some cleaning fluid and then covered with drapes. You will not be able to see the surgery and the spinal block will prevent you from feeling any of the operation.
Some people find listening to music through their headphones to be a good distraction. It helps them to relax, and this will be offered to you. You may wish to bring your own music on your phone or portable music device, and your own headphones. Some people prefer to have a small amount of sedation so that they have a light sleep through their surgery. Your anaesthetist will discuss and agree with you a plan depending on your medical history, and your wishes.
The operation typically takes about 1.5 hours. During this time, your observations will be continually monitored by your anaesthetist.
After the operation
At the end of your operation, you will be transferred to the recovery area where the nurses will monitor your observations. You will be encouraged to eat and drink.
When your spinal anaesthetic has sufficiently worn off, you will be assessed by the therapy team. Our nursing and therapy teams will help you get up, stand, and practice walking with suitable walking aids. The team will practice with you getting on and off the bed, chair, toilet and give advice on how to dress. You will be encouraged to get dressed in home “day clothes” with supportive footwear (no mules or sliders). You will also be taught how to safely complete the stairs.
In order for you to return home, the team needs to be happy that you can manage these activities at home with walking aids. If you require any equipment to assist you this will be assessed and provided prior to your discharge. Please bear this in mind when organising your transport home.
Going home after your operation
Returning home
Everyone reaches their post-operative goals at different times. This determines whether it is safe for us to let you go home on the same day as your operation, or if you need to stay overnight with us at the hospital.
Arrange for someone to collect you
When you have been cleared for discharge, you can contact your family or friends to come and collect you from the hospital.
Arrange for support at home
If you live alone you will need to arrange for a friend or relative to stay with you overnight, post discharge and for a few days after returning home. You should arrange this before you come in to have your surgery.
Wound dressing
Your wound is covered by a shower proof dressing so you can shower as soon as you feel able but do not aim water directly at the dressing. You will be seen by a healthcare professional two weeks after your operation to have your wound checked. Please leave any dressings in place and keep as dry as possible until this appointment.
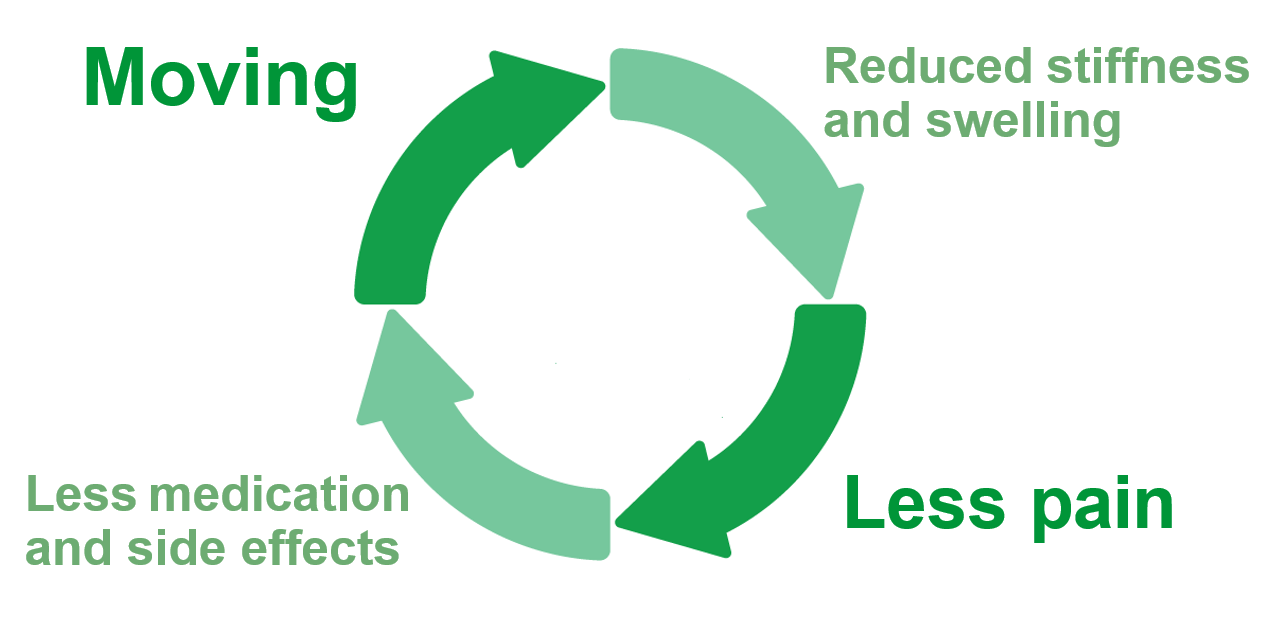
Keep active after your operation
The sooner you can get up and walk after your operation, the better and faster your recovery will be. You will also have a lower risk of complications after your surgery. Keeping still after your operation tends to result in your leg swelling, which ends up making it even more painful to walk. This can cause more side effects, which requires more pain relief, resulting in a vicious circle.
Pain control
Joint replacement surgery is painful – just like any other surgery. The first few weeks can be a difficult period. However, it is important to stay active and keep up with your movement exercises. We will be giving you strong pain relief medication. However, you should expect there to still be mild to moderate pain on movement. It is not going to be 100% pain free.
The pain relief package you receive has been specially designed to try and control your pain as well as possible. It starts from the day of your surgery and continues after your discharge home. We will give you the same pain relief tablets whether you stay in hospital overnight or return home on the same day as your operation.
The pain relief package requires you to take your medicines at specific times.
Additional medications
We will be asking you to take additional medications to help minimise side effects, such as nausea or constipation. Other medications will be given to reduce the chance of certain complications, such as blood clots after your operation. You will be given clear information about the medicines you are sent home with, and when to take the doses.
What to expect when you get home:
Swelling is common to have some generalised swelling of the leg below your hip replacement. Swelling will often get worse if you sit for prolonged periods, so we encourage you to remain gently active. To help reduce lower limb swelling you may need to rest for at least 20 minutes in the morning and / or afternoon on the bed initially. If you experience increasing swelling and pain, please seek medical advice.
Constipation is usually due to the pain relief medication you are taking. We will give you some laxative medication as part of the routine pain relief package. However, please ensure that you take these as prescribed, along with plenty of water to drink. Keeping mobile will also help reduce symptoms. If you struggle, then please discuss this with your GP.
Pain is the biggest issue. It is something you should expect after your operation, but it is key that you do not stop doing your exercises. Please make sure that you follow the pain management programme you were discharged with to help control your pain.
Sleepless nights: It is common for people to experience some disturbance in their normal sleep pattern in the first few weeks after an operation. Please do not worry as this usually improves with time. You can sleep in any position including lying on either side.
What to look out for
Deep vein thrombosis (or DVT) Blood clots in the leg can occur after joint replacement surgery. If your leg becomes hard, swollen, hot and painful, especially in the calf area then this could be a sign of a blood clot. Please seek medical advice if you get these symptoms.
Infection is very rare. However, if your joint replacement or scar becomes hot, red and / or increasingly swollen or if you feel unwell, then please do seek medical assistance.
Support after discharge
The Ward team will let you know what arrangements have been made for your follow-up appointments.
Following your discharge from hospital, there is always someone you can contact for advice.
If you would like more information before your operation or have any questions after you have been discharged home or concerns about your wound, please ring 0117 414 1331 and one of the nursing staff will be able to advise you directly or be able to contact people from your surgical team for you.
For therapy related queries, please contact Physiotherapy admin 0117 414 4412 or Occupational Therapy admin 0117 414 1272.
Physiotherapy advice
Completing the exercises on the following pages will benefit your recovery, improve movement in the hip joint and develop the strength of muscles around it.
These exercises should be completed before and after your surgery. Doing these exercises before your operation will benefit your recovery.
We recommend you continue these exercises for a minimum of 6 weeks post-surgery. Complete your exercises 3 to 4 times a day, repeating each exercise up to 10 times.
Bed exercises
To watch a video of exercises to do in bed visit:
Hip replacement - bed Exercises (youtube.com)
Ankle pumps
Lying on your back, point your toes up and down for the count of ten. Repeat every hour you are awake.
The aim of this exercise is to improve the circulation in the lower limbs, helping to prevent the formation of deep vein thrombosis (blood clots) and reduces swelling.

Knee bracing (static quadriceps)
Lying down on your back with your legs straight.
Pull your ankle up towards you and push the back of your knee down against the bed.
Hold for 5 seconds, then relax.
Repeat 10 times.
The aim of this exercise is to strengthen your thigh muscles ready for standing and walking.

Heel slides (on sliding sheet)
Lying down on your back with your legs straight.
You will need assistance to place sliding sheet under your heel.
Bend and straighten your hip and knee by sliding your foot towards your body and then away.
Repeat 5 – 10 times.
The aim of this exercise is to increase your hip movement.

Hip abduction (on sliding sheet)
Lying down on your back with your legs straight.
You will need assistance to place sliding sheet under your heel.
Slide your leg out to the side and back in.
Repeat 5 – 10 times.
Do not bring your leg back over your body’s midline.
The aim of this exercise is to increase your hip movement and strengthen the surrounding muscles to help with walking.

Bridging
Lying down on your back with your knees bent and feet flat on the bed.
Tense your tummy and bottom muscles and lift your bottom up off the bed.
Hold for 5 seconds.
Repeat 5 – 10 times.
The aim of this exercise is to stabilise your pelvis during walking.

Standing exercises
To watch a video of exercises to do while standing visit:
Hip replacement - standing hip exercises (youtube.com)
Hip flexion in standing
Bend your hip and knee up in front of you and lower back down.
Repeat 5 – 10 times.
The aim of this exercise is to strengthen your muscles at the front of your hip.

Hip extension in standing
Keep your leg straight and take it behind you.
Try not to bend at the hips or knee.
Try to stand up tall.
Repeat 5 – 10 times.
The aim of this exercise is to strengthen your bottom muscles to help with walking.

Hamstring curl in standing
Lift your foot off the floor behind you, bending your knee.
Try not to bend at the hips.
Repeat 5 – 10 times.
The aim of this exercise is to stretch the muscles at the front of your hip and strengthen your muscle on the back of your leg.

Hip abduction in standing
Keep your leg straight and take it out to the side.
Try not to bend at the knee.
Repeat 5 – 10 times.
The aim of this exercise is to strengthen your bottom and hip muscles to help with walking.

Mini squats
Bend both your knees, pushing your bottom out behind you.
Keep your knees behind your feet.
Repeat 5 – 10 times.
Do not bend your hip more than 90 degrees.
The aim of this exercise is to strengthen your leg and hip muscles.

Calf raises
Raise up onto your toes on both feet.
Lower back down onto your flat feet.
Repeat 5 – 10 times.
The aim of this exercise is to strengthen your calf muscles.

Walking
Following your operation, you will be encouraged to get up and walk. It is important to walk on a regular basis and to steadily increase the distance as you recover. It is normal to be allowed to put full weight through your operated leg.
As soon as possible, try and walk placing one foot past the other in a normal walking pattern. You can progress to using one crutch or a stick held on the side opposite to your operated leg as soon as you feel safe and comfortable to do so. If you are uncomfortable or if you limp when walking, continue to use your walking aids.
Stairs
The therapist will practice with you how to safely complete the stairs before going home. To go up and down the stairs, use a banister rail if there is one.
Go up leading with the unoperated leg first, followed by the operated leg and then the crutch.


Going down, put the crutch on the step below then step down with the operated leg, followed by the unoperated leg.
Therapy advice
Activity
Walking is good for your new hip but remember your hip is an artificial joint. Pace your activity, walk and exercise regularly, little and often. The risk of dislocation is greatest in the first six weeks following surgery. To reduce the risk of dislocation whilst the tissues around your hip are healing, avoid forcing or overstretching movements. Avoid the combination of bending the hip and knee across the body towards the opposite shoulder as shown in the picture below.

Sleeping
You may sleep in any position including lying on either side. Initially when you lie on your non-operated side it may be more comfortable with a pillow between your legs to support the operated hip. When getting into bed, position your bottom back towards the centre of the bed and then slide yourself around into bed lifting your legs onto the bed.
Sitting
Sit in a comfortable supportive chair after your operation (ideally with chair arms) to help you get up and down safely. Avoid low soft seating initially after your operation.
Getting dressed
To put pants or trousers over your feet, hold the waistband and lower garment to your feet, inserting the operated leg first followed by the other leg before pulling them up.
To undress, complete in reverse. When putting on shoes and socks, reach down on the inside of the operated leg to avoid uncomfortable twisting of your hip. A long handled reacher, shoehorn and sock aid can make dressing easier. These are readily available from mobility shops, pharmacies and online.
Relationships
It is normal for your sex life to change initially following a joint replacement. Sexual intercourse may be resumed when you feel comfortable.
Driving
You can travel as a passenger in a car immediately following your operation.
- It is best to sit in the front seat, have someone move it well back and reclined
- If possible, get into the car directly from the drive or road rather than the kerb or pavement
- Use your arms to lower yourself onto the edge of the car seat
- Keep your operated leg straight and out in front of you
- Slide back into the seat
- Lift both legs in as your body turns to sit upright in the seat.


You can usually resume driving around four to six weeks after your operation. Stop regularly on longer journeys so you can get out of the car to change position and move around. You must be safe to drive and be able to do an emergency stop.
We recommend that you inform your insurance company you have had a hip replacement before you start driving.
Returning to full activities
Most people are ready to return to work at six to eight weeks after their operation. Air travel should be avoided whenever possible for the first six weeks. Depending on the sensitivity of the security scanner, your hip replacement may set off the alarm.
You can resume most physical activities as soon as you feel comfortable and confident. You can swim once your wound has healed, swimming any stroke including breaststroke. Exercise bikes and treadmills can be used from six weeks, returning to outdoor cycling once comfortable. If you play golf, we suggest you can resume gradually after six weeks.
For activities such as tennis, badminton and cricket we suggest resuming from around 3 months.
Contact sports are not advised following this surgery.
Equipment
The walking aids and any equipment prescribed to you after your surgery are provided by an equipment supplier. Please ring the number on the sticker on the equipment, to discuss its return.
© North Bristol NHS Trust. This edition published April 2024. Review due April 2027. NBT003678.
