This page describes a pleural biopsy procedure. If you have any further questions or concerns, please contact the team who organised your biopsy.
Important information about your procedure
- Please report to your appointment with this information leaflet (see opposite date, time and location). Please ensure you leave enough time for your journey to the hospital.
- Please tell the doctors and nurses looking after you about any medical conditions you have, and bring a list of all the medication you take with you.
- Please tell us if you take any medication to thin the blood – these may need to be stopped before your procedure. See page 4 for more details on when to stop your blood thinners. You must continue to take any other medication as normal.
- If you have been told by your doctor that you may be able to go home the same day after your procedure, please ensure someone is able to bring you into and take you home from the hospital.
- Please seek medical advice if you develop any shortness of breath or increasing chest pain at home after your procedure.
You may be asked to sign and date to confirm that you have read this information in full. You will have the opportunity to discuss any questions you might have about the procedure, or any other aspects of your treatment, with a doctor when you come to hospital for your appointment.
What is an ultrasound guided pleural biopsy?
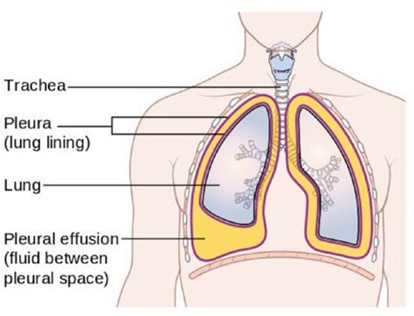
The pleura is a thin membrane that lines the inside of your chest cavity. Some patients have thickening of this lining and require a small sample (a biopsy) be taken to help identify the cause. Before the biopsy is taken, the area will be cleaned and local anaesthetic will be injected to numb the surface of the chest wall. A needle can then be targeted, with the help of an ultrasound machine, to take a biopsy from the pleura. Your doctor may take several biopsies to give you the best chance of a diagnosis. We then analyse these samples in the laboratory to try and get a diagnosis.
Why do I need an ultrasound guided pleural biopsy?
Your doctor has recommended a pleural biopsy as the best way of finding out what is causing your illness. Your doctor will have considered this carefully and made their decision with your best interests in mind. However, it is ultimately your decision as to whether or not you wish to have the procedure done.
If you have any concerns or questions, please let your doctor know and they will be happy to discuss things with you in more detail.
How should I prepare for my pleural biopsy?
Please make sure we have your correct phone number(s) as we may need to call you a few days before your procedure to confirm arrangements and that you are still able to come to hospital. If we are unable to contact you, we may offer your appointment to another patient who is waiting for this procedure.
Please let us know in advance if you are:
- Pregnant.
- Taking medication to thin your blood
If any of these apply to you, we will need to make special arrangements for your procedure. These may include instructions as to what you should do with your medication.
Please bring the following items with you on the day of your procedure:
- All your medications (we need to know what you are taking, including prescription and “over the counter” treatment).
- Reading glasses, if you need them.
What should I do with my medications?
It is important to let us know in advance if you are taking medication to thin the blood. These will need to be stopped temporarily before your procedure can go ahead. Your procedure may need to be cancelled if you do not follow these instructions.
Please take your other medication as normal.
The table below explains what you should do with your medication in more detail. Please contact your doctor if you are not sure what to do. If your blood thinning medication cannot be stopped then your doctor may change it to an alternative medication temporarily, to enable the procedure to take place.
| Medication | Instructions |
|---|---|
| Warfarin | Stop 7 full days before your procedure. You will need to have an INR blood test with your GP or at the hospital 1-2 days before your procedure to make sure your INR is less than 1.5; otherwise we may need to cancel your procedure. |
| Aspirin 75mg | Can continue before your procedure. |
Clopidogrel (Plavix) Dipyridamole (Persantin) Ticagrelor (Brillique) | Stop 7 full days before your procedure. |
Apixaban (Eliquis) Dabigatran (Pradaxa) Edoxaban (Savaysa) Rivaroxaban (Xarelto) | Stop 2 full days before your procedure. |
Dalteparin (Fragmin) Enoxaparin (Clexane) Tinzaparin (Innohep) | Stop 1 full day before your procedure. |
What will happen on the day of my procedure?
You will be greeted by a member of the team who will check your observations (e.g. heart rate, blood pressure, temperature) and go through a checklist with you. This will include questions about your medical history, medications, and allergies.
A member of the team may take some blood for tests if these have not been checked in advance. The procedure itself takes place in a procedure room or theatre. The procedure will be explained to you in more detail, and you will be asked to sign a consent form to confirm you are happy to go ahead.
A doctor will do an ultrasound scan of your chest to help decide where to sample the pleura. This involves placing gel and a hand-held probe over your skin to create a picture on a screen. The ultrasound scan should not be painful and does not involve any radiation. The doctor will then inject local anaesthetic into your chest wall – this may sting at first, but will soon numb the area so you should not feel any pain during the procedure.
Once the area is numb, the doctor will make a small incision and then insert a needle into the pleura to take a sample. Your doctor may take multiple samples from this site to improve the chances of getting an answer. With each biopsy, you will hear a loud ‘click.’ After the samples are taken, a plaster will be placed over the site. There is rarely a need for a stitch.
The whole procedure usually lasts between 30 and 60 minutes in total.
What are the risks of the procedure?
A pleural biopsy is generally a very safe procedure, and serious complications are rare.
- Pain: most people (1 in 2 patients) will experience some pain in association with the procedure, but this is rarely severe. There is likely to be discomfort associated with the local anaesthetic and after the procedure the site may feel bruised. It is normal for your chest to be sore for a week or so after your procedure; this can be managed with simple painkiller (such as paracetamol).
- Infection: there is a low but important risk of infection following a pleural biopsy (less than 1 in 100). This can usually be treated with antibiotics, although it may sometimes need a chest drain to be inserted (a small tube) to empty the chest cavity of any infected fluid and therefore, can result in a hospital stay. Very rarely (1<1000 patients), infections can be more serious and need surgical treatment (an operation). Your doctor will take precautions during the procedure to ensure that this risk is minimised.
- Bleeding: a small amount of bleeding at the site of the procedure is normal. However, a small number of people have significant bleeding during their procedure (1 in 500). This can usually be managed at the time of the procedure, but very rarely another procedure might be required to stop the bleeding (including surgery).
- Pneumothorax (collapsed lung): while your doctor uses the ultrasound scanner to locate the pleura for the procedure, they will also be checking to see where the lung is. However, there is a slight risk that the needle used to take a sample of the pleura punctures the lung, causing it to collapse down. If there is no fluid the risk is around 4 in 100, however this is likely to be much lower in the presence of fluid as in your case. This is called a pneumothorax. This usually doesn’t need any extra treatment but, around 5% of the time a chest drainage tube, pleural vent, or needle will need to be inserted to allow the lung to re-expand. This may require a hospital stay. Even more rarely, if the tube doesn’t fix the pneumothorax, the collapsed lung needs to be treated with a surgical operation.
- Damage to surrounding structures and organs: there is a very small risk that other nearby structures or organs (such as the diaphragm or liver) could be damaged during the biopsy procedure. However, the use of ultrasound to find a suitable and safe site makes this extremely unlikely.
- Failure to get a diagnosis: there is no guarantee that the biopsy will give an overall diagnosis. If the biopsy does not provide an answer as to the cause, your doctor will discuss what further investigations might be needed with you
- Death: the risk of death from an ultrasound guided pleural biopsy is very, very rare indeed (less than 1 in 1000).
What happens after the procedure?
After the procedure a member of the team will take you back to the observation area, where you will have your observations (blood pressure, oxygen levels, heart rate and temperature) checked again. The team will also arrange for you to have a chest X-ray. If you are in any discomfort, we will give you painkillers to manage this. You must let your nurse and/or doctor know if your chest becomes increasingly painful or you feel increasingly short of breath. If you feel well and your chest X-ray is ok you will be allowed to go home. We would expect everything to be completed in around half a day.
When will the results of my procedure be available?
It will take 1-2 weeks for the results of your pleural biopsy to be ready. This is because it takes time for the specimens to be analysed. You will be given an appointment with the team who organised the biopsy to discuss the results with a doctor about 2 weeks after your procedure. Please contact your lead consultant’s secretary one week after your procedure if you have not received an appointment.
How do I contact you?
If you have any questions or concerns, please contact 0117 414 6322 or the team who organised your biopsy.
In the event of an emergency, please contact your on-call GP or NHS 111 for further advice.
Authors:
Dr Helen McDill, Dr Amelia Clive, Dr Rahul Bhatnagar (Respiratory SpR and Consultants, Respiratory Medicine, North Bristol NHS Trust)
Acknowledgements:
Dr Lindsey Taylor, Dr John Corcoran, Dr Cyrus Daneshvar (Consultants, Respiratory Medicine, UHPNT)
© North Bristol NHS Trust. This edition published January 2024. Review due January 2027. NBT003408
