Introduction
This information aims to help guide you through your recovery from gynaecology surgery. Depending on the type of surgery and your condition, it may be performed open (through a cut in your abdomen), laparoscopically (keyhole) or through the vagina.
Length of stay
Some women can go home on the day of the operation but some will go home 1-2 days after their operation.
After your operation
It is recommended that you get out of bed the same day as your operation, this will reduce your risk of blood clots and you are less likely to develop a chest infection. Moving around will also help if you have trapped wind and it encourages your bowel to recover quicker and return to its normal habits. The nursing team will ensure you have adequate pain relief prior to getting out of bed. If your pain is not well controlled, please speak to your nurse.
Breathing exercises
It is important to perform deep breathing exercises after your operation to reduce the risk of developing a chest infection. Do this by taking 3 deep breaths, feeling your lower ribs move. Repeat this every hour throughout the day. If you need to cough after your operation, place a rolled-up towel across your abdomen and apply pressure. If you have had vaginal surgery, put your hand over the pad to support the perineum (the area between your vagina and back passage(anus/ rectum)) when coughing.
Circulation
Regular movement of your legs is essential while you are less active than usual. Move your feet up and down at the ankles for 30 seconds every half an hour when you are in bed or sitting. You will also be given support stockings to wear whilst your mobility is reduced following your operation.
Getting out of bed
Bend your knees up one at a time. Keep knees together and roll onto your side. Push up into sitting with your arms, at the same time lower your legs over the side of the bed. If you have had abdominal surgery you can support your incision with a rolled-up towel.
You can expect pain after your surgery. You will be provided with painkillers on discharge. Some painkillers, such as codeine, can cause constipation. Therefore, make sure to consume a high fibre diet and drink plenty of water to avoid constipation. Taking painkillers to reduce your pain will ensure that you get out of bed sooner and will therefore speed up your recovery and reduce the risk of blood clots.
Packs
You may have a pack (small gauze similar to a tampon) in your vagina following vaginal surgery to reduce the risk of bleeding. This will be removed by a nurse while you are in hospital.
Vaginal bleeding
You may have some vaginal bleeding for 2-3 weeks after your surgery. This is normal. However, if the bleeding becomes heavy or smells offensive, you need to contact your GP or the hospital as this may signify an infection. Use sanitary towels instead of tampons to reduce the risk of infection.
Toileting advice (going to the toilet)
Bladder
You may have a urinary catheter (tube into bladder to help it drain) in place after your operation for up to 24 hours until you are easily able to walk to the toilet to empty your bladder. Once your catheter is removed you can go to the bathroom to empty your bladder.
Ensure you sit on the toilet properly and relax your breathing. If you are struggling to empty your bladder it is important to speak to your nurse. They will measure how much urine you pass (pee) and scan your bladder to determine how much is left.
If you have had a pelvic floor repair especially of the anterior wall of your vagina, you may notice that your urine flow is slower and may take longer. This should settle with time. If you have problems passing urine, you may need to have a catheter for a few days.
It is important to ensure you drink enough after your operation, approximately 1.5 to 2 litres per day, little and often is best. Try to avoid caffeinated drinks, fizzy drinks, and alcohol as these may irritate your bladder and cause urgency. Drinking less frequently can make your urine more concentrated which can irritate your bladder. Also try to avoid going to the toilet ‘just in case’ even if you have fear of leaking as this can lead to poor bladder habits.
Bowels
It is important to avoid constipation after your operation as this puts extra strain on your pelvic floor muscles and potentially your operation site. To prevent constipation, make sure you drink plenty of fluid, increase the fibre content in your diet and if necessary, use laxatives. Your doctor can prescribe these for you to take whilst in hospital and at home.
Sit on the toilet with a stool under your feet, as shown in the picture below. Do not strain and keep your tummy muscles relaxed.
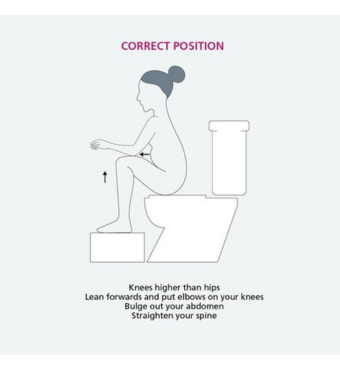
It is helpful to take a slow breath in through your nose so that your stomach moves outwards, and your chest remains still and then exhale through pursed lips. You may also find it useful to support your perineum (the area between your back passage (anus/rectum) and your vagina), when opening your bowels. Please see the picture below.
Exercises
Pelvic floor exercises
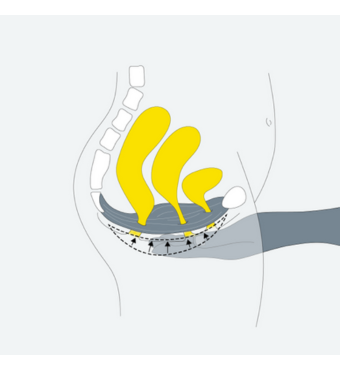
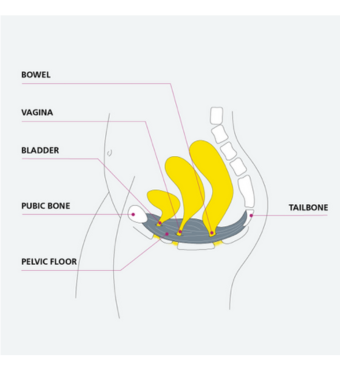
Your pelvic floor muscles are a sling of muscle from the pubic bone at the front of your pelvis to the coccyx and sacrum at the back of your pelvis. They help to support the bowel, bladder and uterus, maintain bladder and bowel control, support the pelvis and aid sexual function.
It is important to strengthen these muscles leading up to and after your operation. Once your catheter has been removed and you can pass urine, you can gently start these exercises.
To contract your pelvic floor, tighten your back passage – as if you are stopping yourself passing wind (farting). At the same time, tighten your vagina. Women used to be told to practice their pelvic floor muscle training by stopping the flow of urine. This is no longer recommended as it can affect your bladder function in the long term.
Try to feel the muscles lifting upwards and forwards towards the pubic bone. Feel the muscles working together. Then relax, let go and feel the muscles return to their starting position. Try not to squeeze your buttocks or leg muscles. Avoid holding your breath and just continue to breathe normally.
To begin with, especially if you haven’t practised these exercises before, you might lack confidence. Keep practicing the above and when you’ve mastered simply contracting and relaxing, move onto the next exercises.
There are two different recommended pelvic floor exercises:
Exercise 1 – Slow pull-ups
Tighten the pelvic floor muscles slowly. Continue to tighten for the length of the hold, relax, and feel the muscle let go. How many seconds can you hold the contraction for?
Aim for 5 seconds to begin with, when you let go – can you feel the muscles relax?
If not, you have held the contraction for too long, try again with a shorter hold – even just one second. Some women may only be able to only hold for 1-2 seconds. Others as many as 8-10 seconds. Don’t panic if you are not able to feel very much to start off with. It may take a bit of practice so keep going. The key is to discover your hold time, and gradually build this up to a maximum of 10 seconds. And don’t forget, keep breathing normally throughout.
Rest for roughly 5 seconds in between each contraction, to ensure that the muscles have fully relaxed. Repeat this 5 times. As it gets easier, gradually increase the length of hold, and number of repetitions (aim for 10 long squeezes for 10 seconds each).
Exercise 2 – Fast pull-ups
Tighten the pelvic floor muscles quickly. Let go straight away. Wait for a second. Repeat this 10 times and as you get more confident aim for approximately 1 contraction per second.
Pelvic floor exercise routine
Do exercise 1 and 2 at each session. As soon as you can, increase to 10 slow and 10 fast pull-ups. Aim to repeat each session at least 3 times a day. When you start, do the exercises lying or sitting. As your muscles get stronger progress to standing.
Do not expect immediate improvement – but do not give up. As the muscles get stronger you will be able to increase your hold time and number of repetitions. Use this link to view our pelvic floor video to help guide you.
How to do pelvic floor exercises - msk (bnssg.nhs.uk)
Top tips
Try to get in the habit of tightening your pelvic floor muscles before you cough, sneeze or lift anything.
Abdominal exercises
After your operation it is important to start strengthening your deep abdominal muscles called tranversus abdominis. They work together with your pelvic floor muscles to provide support for your spine and internal organs.
Deep core muscles
Lying on your back let your tummy relax, breath in gently. As you breathe out gently pull in the lower part of your tummy, hold for 5 seconds, and repeat 5 times. Do not move your back. You should be able to breathe and talk whilst exercising. This can also be done in sitting or standing.

Pelvic tilting
Lie on your back with your knees bent. Pull your tummy in and flatten your back on the bed. Hold, and then relax. Do not hold your breath. Repeat 5-10 times twice daily.
For exercise progressions please visit: POGP (thepogp.co.uk)

General guidelines for returning to activity
It is normal to feel tired after your operation. Everyone recovers at different rates after surgery, but ensuring you have enough rest is important, as well as gradually building-up your activity levels. This will assist your recovery and help reduce post-operative complications. The following table should be used as a general guide.
Laparoscopic surgery
| Healing stage | Activities |
|---|---|
| 0-2 weeks | No heavy lifting for example no heavier than a full kettle Short walks close to home for the first few weeks then gradually increase your distance. Pelvic floor exercises and gentle abdominal exercises. |
| 2-4 weeks | Increase your lifting but still avoiding heavy items. Low impact activity levels, e.g. swimming (ensure bleeding and discharge has stopped). Continue to increase your walking distance. Continue with pelvic floor and abdominal exercises. |
| 4-6 weeks | Return to normal activities, e.g. contact sport or heavy lifting. Continue with pelvic floor exercises. |
Abdominal surgery
| Healing stage | Acitivities |
|---|---|
| 0-2 weeks | No heavy lifting, e.g. no heavier than a full kettle. Short walks close to home for the first few days and then gradually increase your distance. Pelvic floor exercises and gentle abdominal exercises. |
| 2-4 weeks | Gradually increase your activities but avoid heavy lifting. Low impact activities. Continue with pelvic floor and abdominal exercises. |
| 4-6 weeks | Continue gradually increasing your daily activities including lifting. |
| 6+ weeks | Return to normal activities, e.g. contact sport or heavy lifting. Continue with pelvic floor exercises. |
Prolapse surgery
| Healing stage | Activities |
|---|---|
| 0-2 weeks | No heavy lifting, e.g. no heavier than a full kettle. Short walks close to home. Pelvic floor exercises and gentle abdominal exercises. |
| 2-6 weeks | No heavy lifting, e.g. no heavier than a full kettle. Short walks - aim for 30-60 minutes a day to begin with, then gradually increase this as you are able to. Continue with pelvic floor and abdominal exercises. Swimming (ensure bleeding and discharge has stopped). |
| 6-12 weeks | After 6 weeks gradually build up your activity levels. Continue with pelvic floor exercises. |
| 12+ weeks | After three months you should be able to return to all your normal activities, e.g. contact sport/high impact. Avoid unnecessary lifting. Continue with pelvic floor exercises. |
More information
If you are unsure about starting an activity or sport that requires heavy lifting or straining, please discuss with your consultant. For more information on recovering well from laparoscopic/abdominal or vaginal gynaecological surgery please visit the links below:
Recovering well from gynaecological procedures | RCOG
For more information about recovering well from prolapse surgery please use the QR code:
Driving
Do not drive until you are confident you can do an emergency stop. If you have undergone abdominal surgery, we advise you not to drive for at least 4-6 weeks but check with your insurance company regarding your policy.
Sex
You should avoid sexual intercourse for the first 6 weeks following vaginal or hysterectomy surgery, ensuring any bleeding has stopped. This will allow tissues to heal and reduce the risk of developing an infection. It is important that you wait until you feel ready and use sufficient lubrication. If you are concerned or intercourse remains uncomfortable after 3-4 months, it is a good idea to discuss this with your GP.
Useful Resources
BNSSG Pelvic Health Physiotherapy Service : Pelvic Health Physiotherapy Service - msk (bnssg.nhs.uk)
POGP POGP (thepogp.co.uk)
RCOG Home | RCOG
NHS The NHS website - NHS (www.nhs.uk)
Squeezy NHS app for pelvic floor exercises: Home Page - Squeezy (squeezyapp.com)
References
BSUG (2020) Anterior vaginal wall repair without the use of mesh.
IUGA (2020) Recovery Guide Following Vaginal Repair Surgery/Vaginal Hysterectomy
POGP (2019). Fit following Surgery advice and exercise following gynaecological surgery.
RCOG (2015) Information for you after a Laparoscopic Hysterectomy.
RCOG (2015) Information for you after a Pelvic Floor Repair Operation.
RCOG (2015) Information for you after a Vaginal Hysterectomy.
RCOG (2015) Information for you after an Abdominal Hysterectomy.
© North Bristol NHS Trust. This edition published June 2024. Review due June 2027. NBT002353.
